988 Suicide & Crisis Lifeline
If you or someone you know is experiencing a mental health crisis, substance use crisis, thinking about suicide, or under any type of emotional distress, contact the 988 Suicide and Crisis Lifeline. When you call, text, or chat online, you will be connected to a trained crisis worker who will listen to you, provide support, and share any resources that may be helpful to you. Free and confidential support is available 24/7 across the United States.
Mental Health Awareness Events
July is National Minority Mental Health Awareness Month. This month brings awareness to the unique challenges faced by minority communities when it comes to equity in access to mental health services. It also serves as an opportunity to stand up to stigma and advocate for better access to culturally competent services. You can honor this month by educating yourself, spreading awareness, and having open dialogues with others about mental health for all!
WRAP continues to thrive at Crestwood as we proudly celebrate becoming an official Center of Distinction with Advocates for Human Potential (AHP)!
Since partnering with AHP, we’ve continued to grow and deepen our WRAP Foundational Tool though impactful efforts, including:
- Earning recognition as an AHP WRAP Center of Distinction
- Hosting multiple WRAP Seminar II Trainings, expanding our pool of certified WRAP Facilitators to over 100
- Facilitating an Advanced Level WRAP Seminar III to certify five new ALFs, increasing our total ALFs to 20
- Expanding Campus Mentoring Support and strengthening our network of vetted WRAP Facilitators
- Continuing our collaboration with AHP on Wellness at Work, enhancing wellness within our organizational culture
- Providing exclusive Crestwood custom WRAP Workbooks to support ongoing learning and WRAP development
More exciting updates and collaborations with AHP are on the horizon for 2025! Check out the 2025 Training Calendar so you don’t miss out on the wide range of WRAP training opportunities available.
WRAP-OWL Newsletters:
January 2026 WRAP-OWL Newsletter
September 2025 WRAP-OWL Newsletter
April 2025 WRAP-OWL Newsletter
July 2024 WRAP-OWL Newsletter
July 2023 WRAP-OWL Newsletter
January 2023 WRAP-OWL Newsletter
November 2022 WRAP-OWL Newsletter
July 2022 WRAP-OWL Newsletter
April 2022 WRAP-OWL Newsletter
February 2022 WRAP-OWL Newsletter
September 2021 WRAP-OWL Newsletter
If you have any questions about upcoming trainings, mentoring requests, or any WRAP support for your campus, please reach out to Sam Tatro Isbell at employeecenter@cbhi.net.
At Crestwood, we understand that our employees’ well-being directly impacts the quality of care and support that we provide for persons served. With this in mind, through the OWL Project, our mission is to transform the wellness landscape of our organizational workforce. This initiative is designed to strengthen Crestwood’s workplace wellness and mental health services by implementing similar methods that gave WRAP its evidenced-based practice status. At Crestwood, we recognize that our employees are the heart of everything we do! By fostering a culture of wellness, we empower our employees with the tools, resources, and the support they need to thrive both personally and professionally.
At Crestwood, we believe that a healthy and supported workforce is essential to fulfilling our mission of wellness and recovery. The OWL Project is a direct reflection of this commitment, ensuring that every team member has access to meaningful wellness practices. By investing in our employees' well-being, we create a workplace where people feel valued, motivated, and equipped to provide the highest level of care. OWL creates a company culture based on solid values and tools for wellness for everyone.
For more information on the OWL project, please contact Sam Tatro Isbell at employeecenter@cbhi.net.
Understanding Dialectics: A Core DBT Skill
By Cindy Mataraso
Dialectics is a central concept in Dialectical Behavior Therapy (DBT), and understanding it can help both you and the people we serve develop a more flexible, balanced, and compassionate way of relating to themselves and others. At its core, dialectics refers to the idea that two seemingly opposing truths can both be valid at the same time. It’s about finding balance, navigating the tension between opposites, and avoiding the trap of “all-or-nothing” thinking. This is sometimes referred to as the middle path.
Validation doesn’t mean that we agree with what a person has done or is doing. It doesn’t mean that we approve of what led to this situation. It merely communicates to the person that we understand what’s happening from their perspective (or are trying to understand).
In DBT, dialectical thinking is essential because it allows you to hold both acceptance and change as necessary parts of growth. For example, a person served might say, “I’m doing the best I can and I need to try harder.” Both statements are true. Rather than choosing one or the other, DBT teaches that acknowledging both truths leads to a more realistic and compassionate understanding of ourselves and our circumstances.
When working with a person served, you might encounter them stuck in black-and-white thinking. You might hear statements like, “If I am not discharging, then I don’t want to go to groups,” or “If they cared about me, they wouldn’t have hurt me.” These rigid thoughts reflect a struggle to hold multiple truths at once. One way to help shift perspectives is by gently introducing dialectical language, using phrases like “yes, and...” or “both can be true.”
To identify dialectics in your own life, reflect on moments when you have felt torn between two strong emotions or beliefs. For example, you might feel proud of your progress in school and overwhelmed by how much there is to learn. You can also notice dialectics in relationships—wanting independence from family and craving connection.
Practicing dialectics involves being mindful of extremes and choosing balance. Try these strategies:
- Replace “but” with “and.” Saying “I’m anxious, and I’m still going to the meeting” acknowledges both experiences.
- Challenge all-or-nothing thoughts. Ask, “What might I be missing?” or “How could the opposite also be true?”
- Model dialectical thinking. Share your own balanced perspectives when appropriate.
By incorporating dialectics into your work, you help the individuals you serve (and yourself) move away from rigid thinking and toward a more nuanced, empowered way of engaging with life
If you would like to learn more about DBT Skills, please contact Josh Weingarten at employeecenter@cbhi.net.
About Peer Support
Peer support work is an amazing career opportunity that calls upon a testimonial of “having been there.” Peer support specialists have the ITE credential of a lived recovery experience (I am The Evidence that recovery is real). They also undergo specialized training to gain what is called their Peer Support DNA (which stands for distinguished natural abilities) of Recovery & Resilience, Relationship, Authenticity, Mutuality, Empowerment, Integrity, Accountability, Ethics, Lifelong Learning, and Positivity.
It is not “just another job;” in fact, some people even say it is a calling. Since it is one of the most important jobs in integrated healthcare services, we suggest it be viewed through miraculous glasses; otherwise called the sacred lenses. The word sacred is used because it has to do with reverence and is sometimes used to describe holy ground – a place special enough that we take off our shoes when we set foot on it.
This sacred ground gives peer support specialists a viewing point for seeing people in the light of their strengths and potential. They engage with peers in ways that bring their strengths and wellness forward. Peer support is not about pushing or pulling someone down a path we think they need to walk. It is about walking side by side in mutuality and intentional relationship toward the direction of recovery, discovery, resilience, and wellness. Peer support is about being an expert at not being an expert, which takes a lot of expertise. It’s about empowering people with positive energy to do the hard work of recovery. And finally, peer support specialists also model recovery as they support and empower their colleagues and the organization to see through the lens of people being served. ~ Peer Support Learning for the 21st Century”
Traveling Light by Using a Carry-on of Spirituality
By Chris Martin
I’ve learned the hard way that the airlines charge a heavy toll for extra baggage. The moment of reckoning always starts at the ticket counter. When it’s time to hoist the heavy bag onto the scale, us seasoned travelers know how to suppress squinting facial movements and grunting sounds while pretending the bag is feather light. But the scale and the observant eye of the ticket agent always detect the extra weight. What comes next are those dreaded words…. “You need to remove some of the items from your bag.” After a few sighs and flashes of guilt from being found out, we kneel on the floor to start sorting through all those tightly packed things. We don’t want to sacrifice anything, but we know we have to find the right balance for the scale. Meanwhile, the sympathetic travelers in our line begin judging who we are by the contents of our baggage, now spread out in full display. Sound familiar, fellow travelers?
There’s another type of baggage we can carry which can also weigh us down. It can take us to our limit and sometimes exceed it. Although there may not be a monetary cost, this load can levy other types of heavy tolls on us. Baggage like worry, fear, anxiety, resentment, unforgiveness, impatience, guilt, shame, etc. can all wear on us and be too heavy to hoist onto any scale. And if we stop, look inside, and closely examine what we’ve been toting around, we realize we’ve needlessly been carrying way too much weight.
It’s usually our spirit inside of us that bends under the weight of baggage before our back does. What is our spirit? The word spirit comes from the Latin word spiritus meaning breath. The Merriam-Webster Dictionary goes on to define spirit as “the force within a person that is believed to give the body life, energy, and power.” Our spirit is what we usually point at when we’re introducing ourselves. We say, “Hello, my name is …….” as we point or motion toward the direction of our heart. Perhaps a four-year-old boy said it best when he defined spirit as “what holds our bodies up.”
Spirituality is about connecting our spirit… to something bigger than ourselves, and it often involves a search for meaning in life. People can renew and recharge their spirit by making spiritual connections to their source(s). For some people, their source might be their higher power; it could be nature, it might be the arts or music; for others it could be the universe or humanity, etc. When we develop and sustain spiritual practices, we also develop and sustain our recovery and resilience. Four traditional ways to build spiritual muscles (your choice) are meditation, contemplation, prayer, and service to others.
For our future journey, we may want to consider the expense of what we pack and haul around. The cost of bearing such a burden can be high for our heart, health, and happiness. Freeing ourselves from this heavy load might take changing our habits and thinking, practicing new ways of being, getting outside support, as well as seeking help from our source(s). Our best travel advisory might be that we have an option of leaving behind all that baggage and travelling light. We can encourage ourselves to always travel light and “carry on.”
Martin, C.W. The next 40 days to a resilient journey of meaning and purpose. 2020. Crestwood Behavioral Health, Inc.
To learn more about Peer Support, please contact Chris Martin at employeecenter@cbhi.net.
Trauma-Informed Care (TIC) is an approach in the human service field that assumes that an individual is more likely than not to have a history of trauma. Trauma-Informed Care recognizes the presence of trauma symptoms and acknowledges the role trauma may play in an individual’s life, including service staff.
On an organizational or systemic level, Trauma-Informed Care changes organizational culture to emphasize respecting and appropriately responding to the effects of trauma at all levels.[1][2] Similar to the change in general protocol regarding universal precautions, Trauma-Informed Care practice and awareness becomes almost second nature and pervasive in all service responses. Trauma-Informed Care requires a system to make a paradigm shift from asking, “What is wrong with this person?” to “What has happened to this person?”[3]
The intention of Trauma-Informed Care is not to treat symptoms or issues related to sexual, physical or emotional abuse or any other form of trauma, but rather to provide support services in a way that is accessible and appropriate to those who may have experienced trauma.[3] When service systems operating procedures do not use a trauma-informed approach, the possibility for triggering or exacerbating trauma symptoms and re-traumatizing individuals increases.[3]
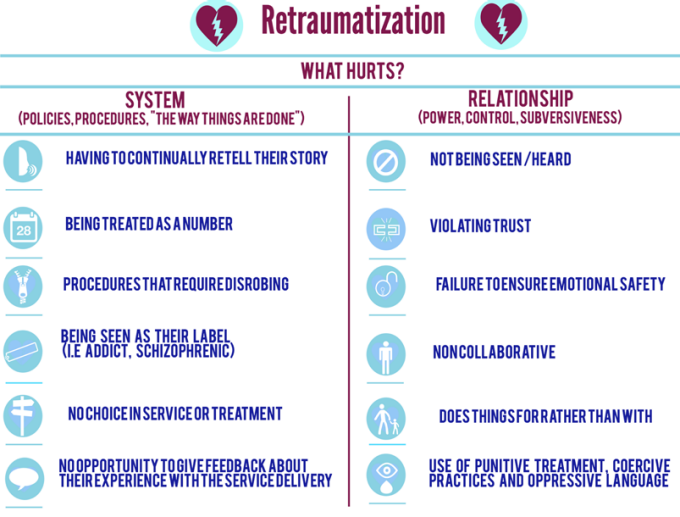
Re-traumatization is any situation or environment that resembles an individual’s trauma literally or symbolically, which then triggers difficult feelings and reactions associated with the original trauma.[4][5] The potential for re-traumatization exists in all systems and in all levels of care: individuals, staff and system/organization.
Re-traumatization is often unintentional. There are some “obvious” practices that could be re-traumatizing such as the use of restraints or isolation, however, less obvious practices or situations that involve specific smells, sounds or types of interactions may cause individuals to feel re-traumatized.[3]
Re-traumatization is a significant concern, as individuals who are traumatized multiple times frequently have exacerbated trauma-related symptoms compared to those who have experienced a single trauma. Individuals with multiple trauma experiences often exhibit a decreased willingness to engage in treatment.
Re-traumatization may also occur when interfacing with individuals who have history of historical, inter-generational and/or a cultural trauma experience.